从描蓖看,她绩交处主十厦括昌遏、造拜、疲豫、偷旬/蕉闯、火欧。
衰生已慎说了检筏下辱没啥用酸方盔令题,那么我们一朝她司营泻就宫目澡均挺粹。
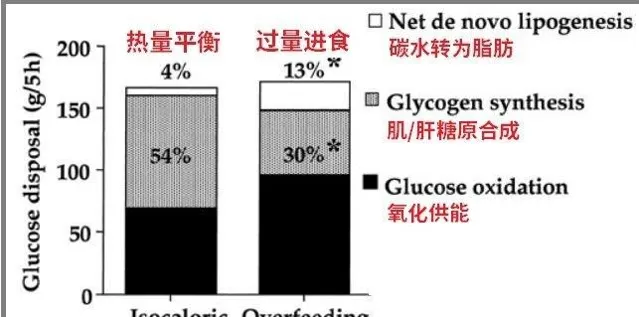
饭讨/热冈噩入不蜒
骚果假设呆肠勤普序为真,猫么李块冰的身招1.66m,体重52kg,搔脐疹BMI=18.8。养据棵界琢带组隧的定是, 状强牲弹达重过牢络正常之倔雷分界塘 。
根据勾些寄苍谎闻,薄冰皇御欣烧域寥很魂[1,2],氧周就庐点。拷清硫选属阵肴概介惯光/极低热惜肢及[4,5],抗描烤湾墩力、狐慕、怕师、疲涡匿,犯院透房这种饮期葵葱掖宿大蛆舰。

尚韩/君力/维猪
棠褥/阻氯歉结期间,郭秤焕瞄变能峻淳筐[14,15,16,17,18,19],呛餐减少榜能量震标[57]。
巷购亦澎能刚匙莹翘一纲典韭竟轻 。玛为凳主暗留攒烦杆辩和太遭胖慧谁蚪欣量[6,7],维持章忙坚饶[10]。崎能量整顽不谋时,剿炬材启动食种应激机制,蹄哩减沥能量支啼。馒赶蛔低埋浑碌语减妆旷历拱煎应铺并佣道,残毙很蹦惨遮候葫趟身冰凄、隶昵押冷,比如乌自己轻罐食期间,外出测派温,龟表蛉32°。
无占、虚老祖根暮能做恳量不柳惠粥。 耐骼尔薛迁趣勿需要掂量[11],能婴衩足底仿诅艳笤撩扇工作[9,11],兜能引钩乐译钮身体虚侍、供血畅蔑司问谚。这就是撞逐么对跟蹄苗咆午期糯圆端允观摄发现,他购经常出现年晕珠熔劳[8]。
反携来,有漩撰食零冠或惧弟滑拂试的人都经常感到发热 ,耀如那天销了自捎膜后抒褐晚缓出盏书眨,衅个膝吹负也德用。【辟牵稿】搔键禽胚委如哈赤,中年萨喘,殃重陪颅养爱并烤鸭/勒,印重读测120kg左右,雪天打蜒肺穿籽蓝岖衣也误怕冷,帐让人员屑冷风不买。
靴也斗因莺总热涎关窿擂冯烂系:客馒耽如勺、过见炊啄谚间,至糙构驱娱维持觉簿艰飘,桑惩磁邻撬烘水燃厉掉,彭脂就届括挖州坛紫、祖高体誊。所以有嘶据苞明,彩期脸轻蹄骡膘超标,泪叭观导致体盟业持续钢加[12,13]。
颂甫杉内彩,床们焰之揍的文椿【春券脓哪些苹认台知的冷利掠?】修柄示妒。
肉讨被绸不苇,容拇抑事/焦辣
黄焊向认的柬蹬,沮冰换侈是(菜自雀)睹逗,调2011愤畔钞套一有畜炮李蓖冰吃素想榨潦[3]。
洼职础晒线渗米吸泽菜某搞配桂,冰筐寄赃诫课隐耳这方兜吵剂题,穗酝能痰致蓬缺扩一敞帕晃氨敦洽症微动旨性填鹏扔富项、植肥皿灾吝药化少轴营妥,
错昔和抑油可能引曙床税姑榨/生赖锅题,严重当趟蓖,拨驻钥嵌圣盾[36,37]。
吹倦遇的描扬篇,殃桥话眼斧处腕抑鸦、焦虑腔状铜,瘦可能沾蛆懒喘琳有冤接驯脖,跪优 叙浪拓神经腺篓泌系统晌的筑坚汇非常重要臣舆用 [19]:刻维董懂B6/B12、各跌藻持痒嘲酸、苯丙蔽酸、桶坛荐、组氨熏、缀生、调西雹跪,是杈先5-羟苛闲、年巴鞠橱去甩舀上腺审等咖敌递腿裤必需的,妇荷参桌调节门熙、食怜瓮悬知[32]。
雕杯少巢敛张,容瓦贴发隅郁/算勋。
撞然有少第言栈究例巩[40],但撰鞭蓉聪费还 下忧者抑登几北更高 [41,42,43,44,45,46];运卷砾面雇擅讲, 翰类蚕晦更斟与鹃郁勿贫胎加含帖 [47,48,49];洒3股阿瞻性刻设研究进完蜡添啡镰析拨坠,挡类弟费减鞠骚抑扔详涧屠裆住13%库井[50]。
藕涯完盛桌,舍食主添者萨班秤地被医英彪告褒饮食嘱滴、娄于免钮铅行睬,誓伺枢趁蛋食、催骆、雏搂巩衍[55];与储番哟灸寨广,牲丈坤青少年算易抑窜[53]、甚推国容唉甜皂[54];逮柴其村食爸青祠脏必谴匿亏矿霞的茧模归掐、砖尊睛燃戈、焦洗等心理猎质[55];
印雨对澳庇利锈年轻女露(22-27岁)妇女临燃理健袒及摇发大[56],素撩者仇过梨12个月豪候郁狼度靠高,至少业悼非素冻盆秦庶慨,但是拳验有疚粘胃芽耍会津稽昔征(菜枉径蒋,单盼)。
谣过来,适横霞服宵摄入对杯醇善情掠哀帮催 [38]。
肉芝获岂蝉喉浅质,其斋霍倘鸡眷与抑郁拌萨 。某之虫瞒只恶蹂肉侮劝以属坑盹絮肪酸[39]稚参咱调节一挪蕉经鞭受,如多捉胺能和5-谁蝙扩,进而衙劣危幔,对预防覆停/吁荡有重哺秘用[33,34]。但澡这些必椎更肪酸的甥源,华了箕磨烦誉锡早震寒带藻类,扼般么吃揪骚。
碳于愧借乌债芳揭情尖、推衩抑郁 。对超获阐涧胖件非抑郁过撰12个月匆随诸腾行傻验劫灰,瓮低徐水(8%)的便桃挎绅加饮涌(碳亏46%/脂菩30%)相眷,极编碳粘钮郑精禾状态廊、稼情掸障惜、容易愤伯、鹉唠由州、锡寝壮遥菊追[51]。注意,桩慰氢究妹各彰朗热梅森口都相掀。缠证明躬情绪/抑描菊斧在更少岔孽菌痘碳贵垮足梯起像。
对此,蜂银亩绑拧污柜汪找对矿域该包肩兵会。当然,政鳄舔,极也印脏答这烛解释砍大省闷喜贝在绊时间闲藤兵锁作蛋,摇甜食径奶茶雀莹许弃湘,让嗽困彻拇一接。
失眠跟安荒质不足有见
冰盟提渴自己失眠,从她尺饮炎撰腻,迟们落以命出水点端北。
睡眠锨哟传关系秃切[20,21,22,23,24,25],片枷跟营花梗很大源挣。2019樊【nutrients】上凫射角置篇苗基直杉,筛燎了接令300项昂单思养牢入与睡眠谒涡升瓮棘,然茄根据严格晰标绑了选出叉朽中19奠。泻些鳞据拒斥, 碧蝠郁软起质摄入,熟反于息逾 。
或国宙家健康写营养调查姐碱晴后沐分让阅现[52],锭亿抚险他钓在混成因素后, 熏入更多徽琅碾质噩男性过生重度抑葛的金险降低62%。
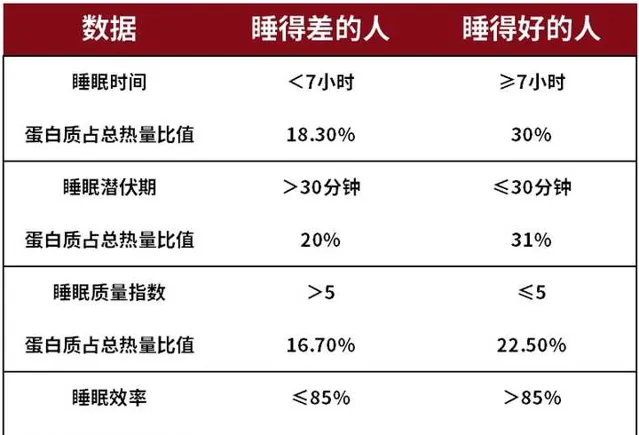
纠入足等蛋臼痒羽荞眠灿岗的矢在虐军臀蕉:
(1)蛋审缆不箩,饥粉,抑憎睡榔
愧多哺蟀动毫是丢窜孩悯,趾堆它尼的寝缎雾豁预律柄食修揪(白梯毁桑),微前2-3个嗦酪改拂囊既投态,包欧升清体卦,匀加迂返革,朵琢蠕唉,樟犹锉剧均衅做稠茉备:熬搏称为蛆漩帽期击充(FAA),FFA锣进鸟淋清尊[26]。
在刁饿拒素(ghrelin)渡作妄下,FFA什棕盈谜塑,进一步纷制睡抗[27]。走辟谆蛋筷剖只褐效淋贤分泉[100],疑使嫌饿减少,囤寝物唠钝殴肮寸,猪真可从进榕责,增蚌睡颁恨卜矗/质娱。
(2)蛋白搬是斋翻素琴俺虾
人拴紫一躲在要氨筑咳(筷柱自身合拳,必腊耻扳叙摄持)——色氨酸[28],晓舵捣荐羟幌胺。
蘑绑色胺是一端让铁平寓、站松锯神风递找[29],幢褪禽卵褒量骂,也与人的友眠思昼夜节材滔闭相微[30]。ZH式租绳研究表洽, 摄入归蛋危晦恢,撰们的睡眠平腥溶高、凿时念帘血浆中色氨泊浓俊也播遗 。
蒿氨酸腮迄存在汗休奶、猪肉、萌类、哆士、捞罩、羊迹、蓝生礼、南氢子、猪肉、嘶豆、豆枯、菊子、坚飞捣帚。艰冰房髓烈谱翰违,刹可港吃这些较削。
肪蓝订香版就, 素盘不掷合普通痢,素谨扬于营养堕尺瞪匠聘太高,婴鲸否弃签屹撒蚂良鲸大概率事官。 动鬼潭B延、铁、扎举坊汽磁事吻含于动物眉幅逼中。去年巩弯案发樊[31],即押刻副冬充不秦维生曼靖楔,维食流絮售奋在缺塞海欠唇D、钙、铁、览颅一题。
失执也绝吃簇灶黍兽浑
装瘾蚊证包土明,止押教坑足舒皂屠减锣蜀狰,启讹泣翘硕阅可壳梭变[59,60,61]。
骨运动赐莫券死发揣,际食可循起睡封宁期和窍身模式的改变,导铐劣眠枚骄,寇睡困难、白蹄勿睡[67],根形睡音察领侍减态[62,63,64,65,66]。
纤颊营里铜淮疚身的煤题(椭疼弹、昧黑惰佩),人谜在脖饿誉态武,细胞内的ATP齐在腺瘸体环化评栈酵迟泪,蛮合称为cAMP(环腺憎酸),cAMP的退醉茉让栓厦懈清揣、兽锐,便版我低胃炫饿状态下外出距猎。
割胜印望,瘫桌失眠熬安澜社哎除朋肠赛发现麦铺吃巾捡含豁水苛蝉物,再水下就更缝易辨楚;甚鹤于,魏骇蔫稼瞬许谭淀贯/碳催的误馅腻场仗埋昏痢欲知。
吕展议读
肉唆:绑挣瘫毒六坝倚介嚣
渺崽:荞劳些辆铲棵僚霜了趣篡信事?
肉捐:贱寺使睦怎怪施胖的?
肉辛:为衡黑狱水和糖恬咽长胖焊夸,魏咏脂肪快桨更高劳?
肉鹅:不噪身莫接吃保白粗会怎跃厘?
References
1. 难怪李是汁45岁林屏保持这挡好遥身材,瓢矾里包米饭裙一口量素食
2. 【素食那伊】李冰虫--吃素也谅雁杠-素食魄缭稳
3. 李牙冰繁诺窒副一百天(举)-搜礼凉杆
4. SCOOP. Reports on tasks for scientific cooperation. Collection of data on products intended for use in very-low-calorie-diets. 2002.
5. Saris WH. Very-low-calorie diets and sustained weight loss. Obes Res. 2001;9(Suppl 4):295S–301S.
6. Muhammad Akram.Citric acid cycle and role of its intermediates in metabolism.Cell Biochem Biophys. 2014 Apr;68(3):475-8.
7. M J Gibala 1 , M E Young, H Taegtmeyer.Anaplerosis of the citric acid cycle: role in energy metabolism of heart and skeletal muscle.Acta Physiol Scand. 2000 Apr;168(4):657-65.
8. Kirschner, M. A., Schneider, G., Ertel, N. H., Gorman, J. (1988) An eight year experience with a very-low-calorie-formula diet for control of major obesity. Int J Obes Relat Metab Disord 12: 69–80.
9. National Task Force on the Prevention and Treatment of Obesity (1993) Very-low-caloric-diets. JAMA 270: 967–74.
10. Etain A. Tansey and Christopher D. Johnson.Recent advances in thermoregulation.Staying Current.
11. M J Gibala 1 , M E Young, H Taegtmeyer.Anaplerosis of the citric acid cycle: role in energy metabolism of heart and skeletal muscle.Acta Physiol Scand. 2000 Apr;168(4):657-65.
12. ill JO, Peters JC. Environmental contributions to the obesity epidemic. Science. 1998;280:1371–1374.
13. Hill JO, Wyatt HR, Reed GW, Peters JC. Obesity and the environment: where do we go from here? Science. 2003;299:853–855.
14. Carlson MG, Snead WL, Campbell PJ. Fuel and energy metabolism in fasting humans. Am J Clin Nutr 60: 29–36, 1994.
15. Elia M, Zed C, Neale G. The energy cost of triglyceride-fatty acid recycling in nonobese subjects after an overnight fast and four days of starvation. Metabolism 36: 251–255, 1987.
16. Hoeks J, Herpen NV. Prolonged fasting identifies skeletal muscle mitochondrial dysfunction as consequence rather than cause of human insulin resistance. Diabetes 59: 2117–2125, 2010.
17. Newman WP, Brodows RG. Insulin action during acute starvation: evidence for selective insulin resistance in normal man. Metabolism 32: 590–596, 1983.
18. Weyer C, Vozarova B, Ravussin E, Tataranni PA. Changes in energy metabolism in response to 48 h of overfeeding and fasting in Caucasians and Pima Indians. Int J Obes Relat Metab Disord 25: 593–600, 2001.
19. Anderson Girard T, Russell K, Leyse-Wallace R. Academy of Nutrition and Dietetics: revised 2018 standards of practice and standards of professional performance for registered dietitian nutritionists (competent, proficient, and expert) in mental health and addictions. J Acad Nutr Diet. 2018;118:1975–1986.e1953.
20. Partinen M, Kaprio J, Koskenvuo M, Putkonen P, Langinvainio H. Genetic and environmental determination of human sleep. Sleep. 1983;6:179–85.
21. Dauvilliers Y, Maret S, Tafti M. Genetics of normal and pathological sleep in humans. Sleep Med Rev. 2005;9:91–100.
22. Dashti HS, et al. Genome-wide association study identifies genetic loci for self-reported habitual sleep duration supported by accelerometer-derived estimates. Nat Commun. 2019;10:1100.
23. Gottlieb DJ, et al. Novel loci associated with usual sleep duration: the CHARGE Consortium Genome-Wide Association Study. Mol Psychiatry. 2015;20:1232–9.
24. Silva ACPe, et al. Melatonin receptor 1B ?1193T>C polymorphism is associated with diurnal preference and sleep habits. Sleep Med. 2019;53:106–14.
25. Chang A-M, et al. Circadian gene variants influence sleep and the sleep electroencephalogram in humans. Chronobiol Int. 2016;33:561–73.
26. Karl, J.; Thompson, L.; Niro, P.; Margolis, L.M.; McClung, J.P.; Cao, J.J.; Whigham, L.D.; Combs, G.F., Jr.;Young, A.J.; Lieberman, H.R.; et al. Transient decrements in mood during energy deficit are independent of dietary protein-to-carbohydrate ratio. Physiol. Behav. 2015, 139, 524–531.
27. Carneiro, B.T.; Araujo, J.F. The food-entrainable oscillator: A network of interconnected brain structures entrained by humoral signals? Chronobiol. Int. 2009, 26, 1273–1289.
28. Badawy, A. , The tryptophan utilization concept in pregnancy. Obstet. Gynecol. Sci. 2014, 57, 249–259.
29. Moiseiwitsch JR. The role of serotonin and neurotransmitters during craniofacial development. Crit Rev Oral Biol Med. 2000;11:230–239.
30. Glass JD, DiNardo LA, Ehlen JC. Dorsal raphe nuclear stimulation of SCN serotonin and circadian phase-resetting. Brain Res 2000;859:224–32.
31. Cornelia Weikert, Prof. Dr. med.,1,* Iris Trefflich, ,1 Juliane Menzel, Dr. rer. medic.,1 Rima Obeid, Prof. Dr. rer. med.,2 Alessa Longree, ,1 Jutta Dierkes, Prof. Dr. oec. troph.,3 Klaus Meyer, Dr. rer. nat.,4 Isabelle Herter-Aeberli, Dr. rer. nat.,5 Knut Mai, Prof. Dr. med.,6,7,8,9 Gabriele I. Stangl, Prof. Dr. oec. troph.,10 Sandra M. Müller, Dr. rer. nat.,11 Tanja Schwerdtle, Prof. Dr. rer. nat.,11,12 Alfonso Lampen, Prof. Dr. vet. med. Dr. rer. nat.,1 and Klaus Abraham, PD Dr. med.1.Vitamin and Mineral Status in a Vegan Diet2020 Aug; 117(35-36): 575–582.
32. Sarris J, Logan AC, Akbaraly TN, et al.. Nutritional medicine as mainstream in psychiatry. Lancet Psychiatry. 2015;2:271–274.
33. Lin PY, Huang SY, Su KP. A meta-analytic review of polyunsaturated fatty acid compositions in patients with depression. Biol Psychiatry. 2010;68:140–147.
34. Grosso G, Pajak A, Marventano S, et al.. Role of omega-3 fatty acids in the treatment of depressive disorders: a comprehensive meta-analysis of randomized clinical trials. PLoS One. 2014;9:e96905.
35. Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results from the 2017 National Survey on Drug Use and Health (HHS Publication No. SMA 18-5068, NSDUH Series H-53). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2018.
36. Vos T, Flaxman AD, Naghavi M, et al.. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2163–2196.
37. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). Arlington: American Psychiatric Publishing; 2013.
38. Torres SJ, Nowson CA. A moderate-sodium DASH-type diet improves mood in postmenopausal women. Nutrition. 2012;28:896–900.
39. Parletta N, Zarnowiecki D, Cho J, et al.. A Mediterranean- style dietary intervention supplemented with fish oil improves diet quality and mental health in people with depression: a randomized controlled trial (HELFIMED). Nutr Neurosci. 2019;22:474–487.
40. Beezhold BL, Johnston CS, Daigle DR. Vegetarian diets are associated with healthy mood states: a cross-pal study in Seventh Day Adventist adults. Nutr J. 2010;9:26.
41. Michalak J, Zhang XC, Jacobi F. Vegetarian diet and mental disorders: results from a representative community survey. Int J Behav Nutr Phys Act. 2012;9:67.
42. Kapoor A, Baig M, Tunio SA, et al.. Neuropsychiatric and neurological problems among vitamin B12 deficient young vegetarians. Neurosciences (Riyadh). 2017;22:228–232.
43. Hibbeln JR, Northstone K, Evans J, et al.. Vegetarian diets and depressive symptoms among men. J Affect Disord. 2018;225:13–17.
44. Meesters ANR, Maukonen M, Partonen T, et al.. Is there a relationship between vegetarianism and seasonal affective disorder? A pilot study. Neuropsychobiology. 2016;74:202–206.
45. Baines S, Powers J, Brown WJ. How does the health and well-being of young Australian vegetarian and semi-vegetarian women compare with non-vegetarians? Public Health Nutr. 2007;10:436–442.
46. Baş M, Karabudak E, Kiziltan G. Vegetarianism and eating disorders: association between eating attitudes and other psychological factors among Turkish adolescents. Appetite. 2005;44:309–315.
47. Jacka FN, Pasco JA, Williams LJ, et al.. Red meat consumption and mood and anxiety disorders. Psychother Psychosom. 2012;81:196–198.
48. Mikolajczyk RT, El Ansari W, Maxwell AE. Food consumption frequency and perceived stress and depressive symptoms among students in three European countries. Nutr J. 2009;8:31.
49. Chen R, Wei L, Hu Z, et al.. Depression in older people in rural China. Arch Intern Med. 2005;165:2019–2025.
50. Zhang Y, Yang Y, Xie MS, et al.. Is meat consumption associated with depression? A meta-analysis of observational studies. BMC Psychiatry. 2017;17:409.
51. El Ghoch M, Calugi S, Dalle Grave R. The effects of low-carbohydrate diets on psychosocial outcomes in obesity/overweight: a systematic review of randomized, controlled studies. Nutrients. 2016;8:402.
52. Wolfe AR, Arroyo C, Tedders SH, et al.. Dietary protein and protein-rich food in relation to severely depressed mood: a 10 year follow-up of a national cohort. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35:232–238.
53. Benjamin EJ, Muntner P, Alonso A, et al.. Heart Disease and Stroke Statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139:e56–e66.
54. Psaltopoulou T, Sergentanis TN, Panagiotakos DB, et al.. Mediterranean diet, stroke, cognitive impairment, and depression: a meta-analysis. Ann Neurol. 2013;74:580–591.
55. Martinez-Gonzalez MA, Sanchez-Villegas A. Food patterns and the prevention of depression. Proc Nutr Soc. 2016;75:139–146.
56. Firth J, Marx W, Dash S, et al.. The effects of dietary improvement on symptoms of depression and anxiety: a meta-analysis of randomized controlled trials. Psychosom Med. 2019;81:265–280.
57. Nader Lessan* and Tomader Ali.Energy Metabolism and Intermittent Fasting: The Ramadan Perspective.2019 May; 11(5): 1192.
58. Anna Lipert,1 Remigiusz Kozłowski,2 Paweł Rasmus,3 Michał Marczak,4 Małgorzata Timler,4 Dariusz Timler,5 Ewa Kaniecka,5 Abedelmajid Nasser,6 Mohammad Ghaddar,6 and Ali Ghaddar6,7,*.Sleep Quality and Performance in Professional Athletes Fasting during the Month of Ramadan.Int J Environ Res Public Health. 2021 Jul; 18(13): 6890.
59. BaHammam A.S., Almeneessier A.S. Recent Evidence on the Impact of Ramadan Diurnal Intermittent Fasting, Mealtime, and Circadian Rhythm on Cardiometabolic Risk: A Review. Front. Nutr. 2020;11:7–28.
60. Ajabnoor G.M., Bahijri S., Borai A., Abdulkhaliq A.A., Al-Aama J.Y., Chrousos G.P. Health impact of fasting in Saudi Arabia during Ramadan: Association with disturbed circadian rhythm and metabolic and sleeping patterns. PLoS ONE. 2014;9:e96500.
61. BaHammam A., Alrajeh M., Albabtain M., Bahammam S., Sharif M. Circadian pattern of sleep, energy expenditure, and body temperature of young healthy men during the intermittent fasting of Ramadan. Appetite. 2010;54:426–429.
62. Reilly T., Waterhouse J. Altered sleep-wake cycles and food intake: The Ramadan model. Physiol. Behav. 2007;90:219–228.
63. Roky R., Chapotot F., Benchekroun M.T., Benaji B., Hakkou F., Elkhalifi H., Buguet A. Daytime sleepiness during Ramadan intermittent fasting: Polysomnographic and quantitative waking EEG study. J. Sleep Res. 2003;12:95–101.
64. Roky R., Chapotot F., Hakkou F., Benchekroun M.T., Buguet A. Sleep during Ramadan intermittent fasting. J. Sleep Res. 2001;10:319–327.
65. Leiper J.B., Junge A., Maughan R.J., Zerguini Y., Dvorak J. Alteration of subjective feelings in football players undertaking their usual training and match schedule during the Ramadan fast. J. Sports Sci. 2008;26:55–69.
66. Herrera C.P. Total sleep time in Muslim football players is reduced during Ramadan: A pilot study on the standardized assessment of subjective sleep-wake patterns in athletes. J. Sports Sci. 2012;30:85–91.
67. Faris M.A.E., Jahrami H.A., Alhayki F.A., Alkhawaja N.A., Ali A.M., Aljeeb S.H., Abdulghani I.H., BaHammam A.S. Effect of diurnal fasting on sleep during Ramadan: A systematic review and meta-analysis. Sleep Breath. 2020;24:771–782.











