
一、主要的好處是活命,降低死亡率
可能有些同學會不解,難道人的死亡率不是100%?還有人可以不死?
其實,在相關科學研究中,死亡是有 時間和物件限制 的。比如我們找來100個中年人,追蹤他們15年,15年內有X人死亡,以此計算死亡率。死亡率在很大程度上反映疾病狀況、生存品質和幹預手段的有效性。
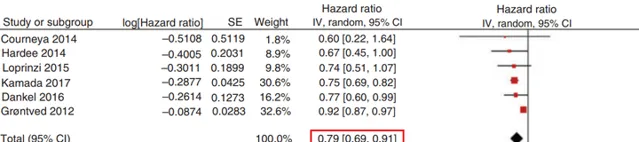
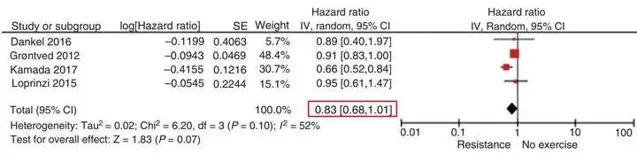
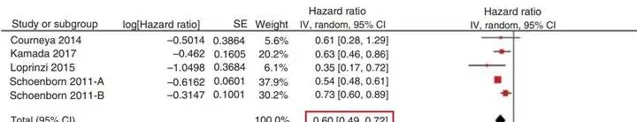
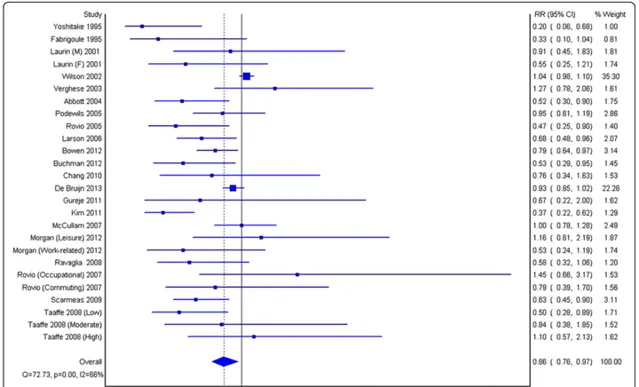
2018年的一項大型元分析包含了 37萬多名參與者 ,平均隨訪9年,年齡18-75歲。主要發現包括:長期進行系統阻力訓練可以 降低21%全因死亡率、17%心血管疾病死亡率 ;如果搭配有氧運動進行可降低全因死亡率40%。
支持肌肉/力量與死亡率之間負相關性的證據堆積如山 。
2008年的一項前瞻性佇列研究,對8762名20至80歲男性[67]追蹤了19年之久,發現肌肉力量與各種原因的 死亡和癌癥呈獨立負相關 ,即使調整了其他混雜因素之後也是如此。年齡調整後,肌肉力量和心肺功能水平高的男性,死亡率比肌力水平最低的不健康男性死亡率低60%。並且,肌肉力量升高是長期訓練的結果[68,69],長期抗阻訓練對死亡率將降低發揮了一定的保護作用。
2007年的流行病學研究調查了800名65歲以上老人[74],發現握力較高男性死亡風險為低19%、心血管風險低27%、癌癥死亡風險低19%,這些關聯在進一步調整了純肌肉量或體脂水平後仍具有統計學意義。
日本廣島成人健康研究(AHS)佇列研究了35至74歲的4912人[75],握力每增加5公斤,男性心臟病風險降低15%、中風風險降低10%、肺炎風險降低15%;即使經過20多年的隨訪,每增加5公斤握力仍然降低相對風險8%。
一計畫美國研究包含了2488名65歲及以上的墨西哥裔美國男性和女性[76],發現在控制了相關的危險因素後,握力是老年墨西哥裔美國人死亡的一個強有力的預測因素,握力<22.01 kg的男性和握力小於14 kg的女性5年後死亡的比例分別為38.2%和41.5%。
對82名老年女性患者的研究發現,最大握力是否達到5KG,是患者存活/死亡的最明確、最敏感分界線[70];日本的一項對6259人的研究發現,跳躍能力/握力/仰臥起坐能力較低的男性具有面臨較高的死亡風險[71];
Metter等人在25年中搜集了1071名男性的數據,握力下降與死亡率增加有關[72];一項對8116人的調查發現,握力/仰臥起坐/伏地挺身等肌肉力量指標可以加拿大人的死亡率[73];
許多研究選擇握力作為測試方式的原因是,它不需要太多的技巧,簡單易行。如果選擇其他運動來測試,則技巧可能會混淆測試數據。
二、肌肉訓練降低死亡率的其中一種機制:對抗腹部肥胖/代謝症候群
數據表明,人類在25至65歲之間,內臟脂肪可增加 300%以上 [9]。
不同部位脂肪的生理效應截然不同[10],腹部/內臟脂肪比總脂肪與代謝症候群的關聯性更強、更容易引發健康問題[11,12,24,25,26,27,28,29,30,31,32,33,35,36,37,38,39]。
但如果脂肪分布在下半身或大腿,則相應風險降低[7,8,13,14,15,16,17,18,19,20,21,22,23]。作為印證,女性的雌激素水平比男性更高,由於雌激素具有減少內臟/腹部脂肪(「轉移」到腿臀部)的作用[34],因此女性的心血管疾病率[34,40,41,42,43]和2型糖尿病機率要低於男性,並且即便兩性的身體脂肪總量大致相等時,也是如此[44,45]。
代謝症候群包含了哪些?
腹部肥胖、血糖/血脂/血壓/低密度脂蛋白膽固醇升高、胰島素抵抗、慢性炎癥,乃至於糖尿病等。並不是胖就完了,代謝症候群其病情發展的終點是各類 致命性疾病 [78,79,80],包括動脈粥樣硬化[47]、心肌梗死[48,49,52]、冠心病[50,51,53]。
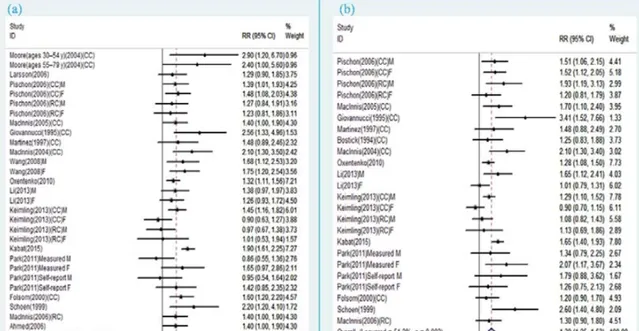
腹部肥胖還促進多種癌癥發病率升高,包括乳癌[81]、結直腸癌[82,90,91,92]、子宮內膜癌[83]、食道癌[86]、腎癌[84]、肺癌[89]、胰臟癌[85]、甲狀腺癌[87]和膽囊癌[88]等。
腰圍越大,各類癌癥機率相應升高。
練肌肉有助於抵抗腹部肥胖和代謝症候群。
因為從原理上說,骨骼肌是人體處理葡萄糖的主要器官[55],在正常情況下它處理了人體大約80%的葡萄糖[56,57]。
骨骼肌是一個巨大的糖庫,普通人的骨骼肌大概能容納400g左右葡萄糖,或者是每kg肌肉12g左右的糖——如果肌肉量很大,或者長期進行大運動量,肌肉可容納的糖甚至可以超過800g。
註意,葡萄糖一旦被運輸進入骨骼肌,被成肌糖原[122],就永遠留在裏面了。因為肌肉中沒有相應的酶(葡萄糖-6-磷酸酶),所以肌糖原是無法分解成葡萄糖重新回到血液,不可能再被合成為身體其他部位的脂肪讓我們發胖。
但隨年齡增加身體老化,人類的骨骼肌逐漸萎縮,30歲後每10年萎縮3-8%[1,2],70歲後每十年就有減少25%-40%[65,66],這導致靜息代謝率降低、葡萄糖攝取減少、脂質氧化能力降低[6]。
已經證明,肌肉的胰島素敏感性、肌肉攝取/利用/消耗血糖的能力(特別是在不依賴胰島素的情況下),與代謝症候群[58,59,60,61,62]和2型糖尿病[63,64]密切相關。
2007年,美國心臟協會臨床心臟病學委員會和營養、體育和代謝理事會發表了一份科學聲明,參照了一項包括8570名年齡在20-75歲之間的男性進行的研究。
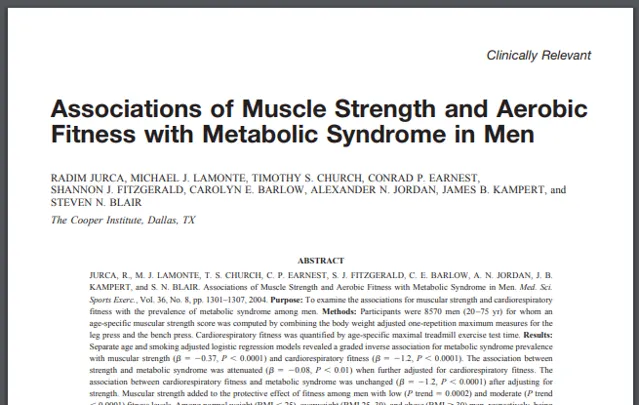
該聲明支持持一切有、無心血管疾病/代謝症候群的人進行肌肉訓練 [93],因為肌肉力量的發展可能會帶來獨立於心血管健康的、額外的好處;肌肉力量與代謝症候群患病率具有獨立負相關關系。
肌肉訓練與有氧訓練帶來的健康益處出在機制上的相似性,包括減少腹部脂肪[94]、降低血液甘油三酯[95]、降低高密度脂蛋白膽固醇[96]、血糖改善等[97]。
無氧運動/抗阻訓練/高強度訓練都對於減少腹部/內臟脂肪有好處。
Treuth等人觀察到對14名健康老年婦女(平均年齡67歲)進行每周3次持續16周的訓練後,她們的內臟脂肪從143減少到130cm²、同時力量和肌肉橫截面積增加[98],研究者認為這些變化對於預防與年齡相關的腹部脂肪增加、及由此帶來的負面健康結果可能很重要。
一計畫中國的研究,針對60名65-75歲的肥胖老人,發現單純的力量訓練能減少老人的內臟脂肪,增加他們的肌肉體積、握力[99]。

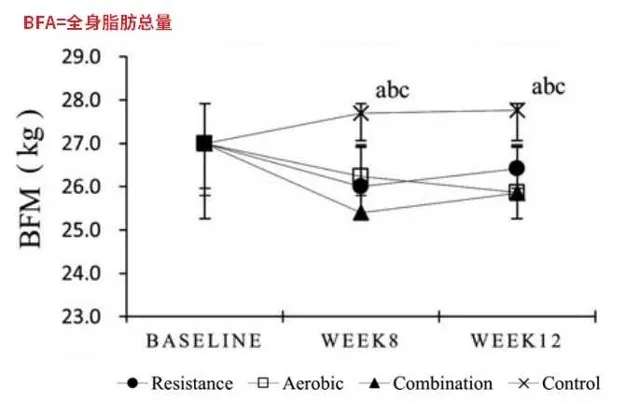
雖然單純抗阻訓練的減脂效果要低於有氧或混合訓練,但也是不可忽視的一種促進健康的手段。而且力量訓練組的老人具有更高的IGF-1水平,這可能導致他們的骨骼、韌帶、關節更健康,代謝狀態最佳化。
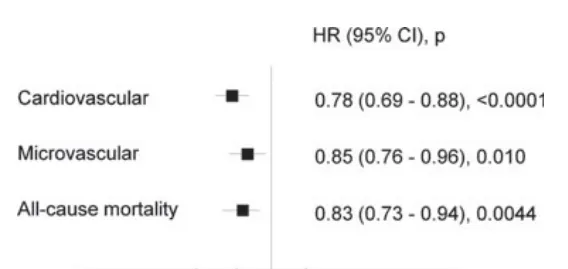
無氧運動/高強度運動在相同的能量消耗下,比有氧運動產生更大的腹部脂肪減少[98]。Blomster等人研究了11140名糖尿病患者,發現與不進行或輕度運動的患者相比,中度至劇烈運動的患者發生心血管事件的風險降低22%、微血管並行癥少15%、全因死亡率降低17%。
所以不難理解為什麽美國運動醫學院推薦超重/肥胖者也進行抗阻訓練[100]。
三、肌肉訓練的更大意義體現在生命力薄弱、身體差的老年人身上
例如抑郁癥,一種嚴重降低生活品質的疾病,許多抑郁癥患者 自殺 [101,102,103,104]。體力活動可以可以提升身體活力,改善生活品質,對抗抑郁癥[105,106,107,108];抗阻訓練也被證明有助於降低抑郁程度[109,110]。
老年人容易發生大腦功能衰退,許多大型研究表明肌肉力量和大腦功能具有密切關系,肌肉力量較強者的反應、邏輯、記憶、認知能力都更高[112,113,114,115,116]。肌肉力量強和大腦功能好兩者之間並不只是單純的同時發生,也有 明確的因果關系 。
Mavros等人設計了雙盲/雙假實驗研究了100名55歲以上患有輕度認知障礙的老人[111],在專業培訓師的監督下,他們進行的為期6個月的漸進負荷力量訓練(負荷為80-92%的大強度)。訓練提高了老人的力量和認知能力,他們的阿茨海預設知表中的得分顯著改善。特別值得一提的是,Mavros等人還研究並排出了肌肉力量與認知之間的反向因果關系, 確認了是肌肉力量提高了認知水平 。
這樣的研究結論被一而再再而三的復制、被反復論證。
Roberta對65歲以上老人進行3個月的漸進力量訓練,方案包括腿屈伸、腿彎舉、臥推、劃船、箭步蹲、拉伸、自重訓練等,促進了他們神經功能和執行能力的改善[117];
Carla等人對67名55-75歲的健康老年人進行16周的力量訓練,在進行思維任務期間,他們大腦左前額葉皮層耗氧量下降,運動訓練使大腦皮層啟用時的腦氧合效率更高,認知表現(反應時間)得到改善[118];
Lindsay等人對86名70至80歲的婦女進行了為期6個月的隨機對照試驗,發現每周兩次的力量訓練可以改善她們的註意力、選擇性、聯想記憶功能,而平衡和協調性訓練則不能[119];
Fia等人100名患有輕度認知障礙的老年人[121],6個月的力量訓練改善阿茨海默平分表48%、無阻力訓練改善27%、認知訓練則無改善只減輕了記憶力的下降。
Tsai等人從大學醫院阿茨海默研究中心招募了66名患有認知障礙的老年人(60至80歲)進行實驗,證實有氧/力量訓練後他們的認知改善,反應時間縮短[120]。
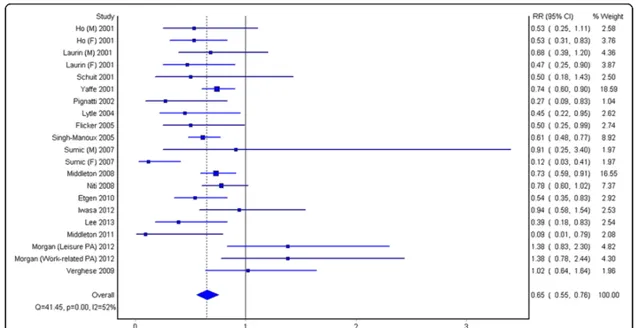
在更宏觀的層面上,Sarah等人對47個列隊研究進行了 元分析 ,得出體力活動與認知能力下降和癡呆呈顯著的負相關關系。體力活動與認知障礙風險減少35%、癡呆風險14%有關;
這些內容我以前寫過,就不詳細鋪開了。
如何看待中國老年人健身很少進行力量訓練,而是采取快走等有氧耐力運動?
此外,肌肉訓練防止摔倒骨折等。對於老年人來說,一次摔倒引發的骨折,結果可能是住院、臥床、喪失行動能力、健康狀況惡化、乃至死亡,網傳袁老就是在一次摔倒後身體狀況急劇惡化的。
此外,就算沒有骨折,長期力量訓練也有助於減少受傷機率和降低傷情,因為負重可導致骨密度提高、韌帶、肌腱、肌肉的韌性/彈性加強。
References
1. Roubenoff R, Castaneda C. Sarcopenia—understanding the dynamics of aging muscle. Journal of the American Medical Association. 2001;286(10):1230–1231.
2. Lexell J, Taylor CC, Sjostrom M. What is the cause of the ageing atrophy? Total number, size and proportion of different fiber types studied in whole vastus lateralis muscle from 15- to 83-year-old men. Journal of the Neurological Sciences. 1988;84(2-3):275–294.
3. DeFronzo R.A., Jacot E., Jequier E., Maeder E., Wahren J., Felber J.P. The effect of insulin on the disposal of intravenous glucose. Results from indirect calorimetry and hepatic and femoral venous catheterization.Diabetes.1981;30:1000–1007.
4. Defronzo RA, Simonson D, Ferrannini E, Barrett E. Insulin resistance: a universal finding in diabetic states. Bull Schweiz Akad Med Wiss. 1981:223–238.
5. Ferrannini E, Simonson DC, Katz LD, Reichard G, Jr, Bevilacqua S, Barrett EJ, Olsson M, DeFronzo RA. The disposal of an oral glucose load in patients with non-insulin-dependent diabetes.Metabolism.1988;37:79–85.
6. Srikanthan P, Hevener AL, Karlamangla AS. Sarcopenia exacerbates obesity-associated insulin resistance and dysglycemia: findings from the national health and nutrition examination survey III. PLoS ONE. 2010;5(5)e10805
7. Snijder MB, Dekker JM, Visser M, Bouter LM, Stehouwer CD, Yudkin JS, et al. Trunk fat and leg fat have independent and opposite associations with fasting and postload glucose levels: The Hoorn Study. Diabetes Care.2004;27:372–377.
8. Snijder MB, Visser M, Dekker JM, Goodpaster BH, Harris TB, Kritchevsky SB, et al. Low subcutaneous thigh fat is a risk factor for unfavourable glucose and lipid levels, independently of high abdominal fat. The Health ABC Study. Diabetologia. 2005;48:301–308.
9. Hunter GR, Lara-Castro C, Byrne NM, Zakharkin SO, St-Onge MP, Allison DB. Weight loss needed to maintain visceral adipose tissue during aging. International Journal of Body Composition Research. 2005;3:55–61.
10. Williams MJ, Hunter GR, Kekes-Szabo T, Snyder S, Treuth MS. Regional fat distribution in women and risk of cardiovascular disease. American Journal of Clinical Nutrition. 1997;65(3):855–860.
11. Peiris AN, Sothmann MS, Hoffmann RG, et al. Adiposity, fat distribution, and cardiovascular risk. Annals of Internal Medicine. 1989;110(11):867–872.
12. Williams MJ, Hunter GR, Kekes-Szabo T, Snyder S, Treuth MS. Regional fat distribution in women and risk of cardiovascular disease. American Journal of Clinical Nutrition. 1997;65(3):855–860.
13. Snijder MB, Zimmet PZ, Visser M, Dekker JM, Seidell JC, Shaw JE. Independent and opposite associations of waist and hip circumferences with diabetes, hypertension and dyslipidemia: The AusDiab Study. Int J Obes Relat Metab Disord. 2004;28:402–409.
14. Kahn HS, Austin H, Williamson DF, Arensberg D. Simple anthropometric indices associated with ischemic heart disease. J Clin Epidemiol.1996;49:1017–1024.
15. Terry RB, Stefanick ML, Haskell WL, Wood PD (1991) Contributions of regional adipose tissue depots to plasma lipoprotein concentrations in overweight men and women: possible protective effects of thigh fat. Metabolism 40:733–740
16. Snijder MB, Dekker JM, Visser M et al (2003) Larger thigh and hip circumferences are associated with better glucose tolerance: the Hoorn study. Obes Res 11:104–111
17. Snijder MB, Dekker JM, Visser M et al (2003) Associations of hip and thigh circumferences independent of waist circumference with the incidence of type-2 diabetes: the Hoorn Study.Am J Clin Nutr 77:1192–1197
18. Lissner L, Bjorkelund C, Heitmann BL, Seidell JC, Bengtsson C (2001) Larger hip circumference independently predicts health and longevity in a Swedish female cohort. Obes Res 9:644–646
19. Van Pelt RE, Evans EM, Schechtman KB, Ehsani AA, Kohrt WM (2002) Contributions of total and regional fat mass to risk for cardiovascular disease in older women. Am J Physiol Endocrinol Metab 282:E1023–E1028
20. Seidell JC, Han TS, Feskens EJ, Lean ME. Narrow hips and broad waist circumferences independently contribute to increased risk of non-insulin-dependent diabetes mellitus. J Intern Med. 1997;242:401–6.
21. Seidell JC, Perusse L, Despres JP, Bouchard C. Waist and hip circumferences have independent and opposite effects on cardiovascular disease risk factors: the Quebec Family Study. Am J Clin Nutr. 2001;74:315–21.
22. Lissner L, Bjorkelund C, Heitmann BL, Seidell JC, Bengtsson C. Larger hip circumference independently predicts health and longevity in a Swedish female cohort. Obes Res. 2001;9:644–6.
23. M.B. Snijder, J.M. Dekker, M. Visser, L.M. Bouter, C.D. Stehouwer, P.J. Kostense, et al., Associations of hip and thigh circumferences independent of waist circumference with the incidence of type 2 diabetes: the Hoorn Study, Am.J. Clin. Nutr. 77 (2003) 1192–1197.
24. 1 Bjorntorp P. Metabolic implications of body fat distribution.Diabetes Care 1991; 14: 1132±1143.
25. Kissebah AH, Videlingum N, Murray R, et al. Relation of body fat distribution to metabolic complications of obesity. J Clin Endocrinol Metab 1982;54:254-60.
26. Abate N, Garg A, Peshock RM, StrayGundersen J, Grundy SM. Relationships of generalized and regional adiposity to insulin sensitivity in men. J Clin Invest 1995;96: 88-98.
27. Planas A, Clará A, Pou JM, et al. Relationship of obesity distribution and peripheral arterial occlusive disease in elderly men. Int J Obesity 2001;25:1068–70.
28. Kete I, Mariken, Volman M, et al. Superiority of skinfold measurements and waist over waist-to-hip ratio for determination of body fat distribution in a population-based cohort of Caucasian Dutch adults. Eur J Endocrinol 2007;156:655–61.
29. Alexander JK. Obesity and coronary heart disease. Am J Med Sci 2001;321:215–24.
30. Willett WC, Manson JE, Stampfer MJ, et al. Weight, weight change, and coronary heart disease in women: risk within the ‘normal’ weight range. JAMA 1995;273:461–5.
31. Goodpaster BH, Krishnaswami S, Harris TB, et al. Obesity, regional body fat distribution, and the metabolic syndrome in older men and women. Arch Intern Med 2005;165:777–83.
32. Garrison RJ, Higgins MW, Kannel WB. Obesity and coronary heart disease. Curr Opin Lipidol 1996;7:199–202.
33. Lakka HM, Lakka TA, Tuomilehto J, Salonen JT. Abdominal obesity is associated with increased risk of acute coronary events in men. Eur Heart J 2002;23:706–13.
34. Lemer D J, Kannel WB (1986) Patterns of coronary heart diseases morbidity and mortality in the sexes: a 26-year followup of the Framingham population. Am Heart J 11:383-390
35. Sparrow D, Borkan GA, Gerzof SG, Wisniewski C, Silbert CK. Relationship of fat distribution to glucose tolerance: Results of computed tomography in male participants of the Normative Aging Study. Diabetes. 1986;35:411–415.
36. Bergstrom RW, Newell–Morris LL, Leonetti DL, Shuman WP, Wahl PW, Fujimoto WY. Association of elevated fasting C-peptide level and increased intra-abdominal fat distribution with development of NIDDM in Japanese-American men. Diabetes. 1990;39:104–111.
37. Nagaretani H, Nakamura T, Funahashi T, Kotani K, Miyanaga M, Tokunaga K, et al. Visceral fat is a major contributor for multiple risk factor clustering in Japanese men with impaired glucose tolerance. Diabetes Care. 2001;24:2127–2133.
38. McNeely MJ, Boyko EJ, Shofer JB, Newell–Morris L, Leonetti DL, Fujimoto WY. Standard definitions of overweight and central adiposity for determining diabetes risk in Japanese Americans. Am J Clin Nutr. 2001;74:101–107.
39. Nakamura T, Tokunaga K, Shimomura I, Nishida M, Yoshida S, Kotani K, et al. Contribution of visceral fat accumulation to the development of coronary artery disease in non-obese men. Atherosclerosis. 1994;107:239– 246.
40. Wingard DL, Suarez L, Barrett-Connor E (1983) The sex differential in mortality from all causes and ischemic heart disease. Am J Epidemio1117:165-172
41. Freedman DS, Jacobsen S J, Barboriak JJ et al. (1990) Body fat distribution and male/female differences in lipids and lipoproteins. Circulation 81:1498-1506
42. Larsson B, Bengtsson C, Bj6rntorp Pet al. (1992) Is abdominal body fat distribution a major explanation for the sex difference in the incidence of myocardial infarction? Am J Epidemio1135: 266-273
43. Seidell JC, Cigolini M, Charzewska Jet al. (1991) Fat distribution and gender differences in serum lipids in men and women from four European communities. Atherosclerosis 87:203-210
44. Despr6s JP, Allard C, Tremblay A, Talbot J, Bouchard C (1985) Evidence for a regional component of body fatness in the association with serum lipids in men and women. Metabolism 34:967-973
45. Krotkiewski M, Bj6rntorp P, Sj6strOm L, Smith U (1983) Impact of obesity on metabolism in men and women. Importance of regional adipose tissue distribution. J Clin Invest 72: 1150-1162
46. Lear S. A., Humphries K. H., Kohli S., Chockalingam A., Frohlich J. J., Birmingham C. L. Visceral adipose tissue accumulation differs according to ethnic background: results of the Multicultural Community Health Assessment Trial (M-CHAT) The American Journal of Clinical Nutrition. 2007;86(2):353–359.
47. McGill H. C., Jr., McMahan C. A., Herderick E. E., et al. Obesity accelerates the progression of coronary atherosclerosis in young men. Circulation. 2002;105(23):2712–2718.
48. Fager G, Wiklund O, Olofsson SO, Wilhelmsen L, Bondjers G (1981) Multivariate analyses of serum apolipoproteins and risk factors in relation to acute myocardial infarction. Arteriosclerosis 1:273-279
49. Hamsten A, Walldius G, Dahlen G, Johansson B, De Faire U (1986) Serum lipoproteins and apolipoproteins in young male survivors of myocardial infarction. Atherosclerosis 59: 223-235
50. Gordon DJ, Probstfield JL, Garrison RJ et al. (1989) Highdensity lipoprotein cholesterol and cardiovascular disease. Four prospective American studies. Circulation 79:8-15
51. Assmann G, Helmut S (1992) Relation of high-density lipoprotein cholesterol and triglycerides to incidence of atherosclerotic coronary artery disease (the PROCAM experience). Am J Cardio170:733-737
52. Austin MA, Breslow JL, Hennekens CH, Buring JE, Willett WC, Krauss RM (1988) Low-density lipoprotein sub class patterns and risk of myocardial infarction. JAMA 260:1917- 1921
53. Crouse JR, Parks JS, Schey HM, Kahl FR (1985) Studies of low density lipoprotein molecular weight in human beings with coronary artery disease. J Lipid Res 26:566-574
54. Bouchi R., Fukuda T., Takeuchi T., Minami I., Yoshimoto T., Ogawa Y. Sarcopenia is associated with incident albuminuria in patients with type 2 diabetes: A retrospective observational study. J. Diabetes Investig. 2017;8:783–787.
55. DeFronzo R.A., Jacot E., Jequier E., Maeder E., Wahren J., Felber J.P. The effect of insulin on the disposal of intravenous glucose. Results from indirect calorimetry and hepatic and femoral venous catheterization.Diabetes.1981;30:1000–1007
56. Defronzo RA, Simonson D, Ferrannini E, Barrett E. Insulin resistance: a universal finding in diabetic states. Bull Schweiz Akad Med Wiss. 1981:223–238.
57. Ferrannini E, Simonson DC, Katz LD, Reichard G, Jr, Bevilacqua S, Barrett EJ, Olsson M, DeFronzo RA. The disposal of an oral glucose load in patients with non-insulin-dependent diabetes.Metabolism.1988;37:79–85.
58. Rabol R., Petersen K.F., Dufour S., Flannery C., Shulman G.I. Reversal of muscle insulin resistance with exercise reduces postprandial hepatic de novo lipogenesis in insulin resistant individuals.Proceedings of the National Academy of Sciences of the United States of America.2011;108:13705–13709
59. R. A. DeFronzo, D. Tripathy, Skeletal muscle insulin resistance is the primary defect in type 2 diabetes. Diabetes Care 32 (suppl. 2), S157–S163 (2009)
60. G. S. Hotamisligil, P. Arner, J. F. Caro, R. L. Atkinson, B. M. Spiegelman, Increased adiposetissue expression of tumor necrosis factor-alpha in human obesity and insulin resistance. J. Clin. Invest. 95, 2409–2415 (1995).
61. M. N. Rao, T. C. Neylan, C. Grunfeld, K. Mulligan, M. Schambelan, J.-M. Schwarz, Subchronic sleep restriction causes tissue-specific insulin resistance. J. Clin. Endocrinol. Metab. 100, 1664–1671 (2015).
62. L. N. Bell, J. M. Kilkus, J. N. Booth III, L. E. Bromley, J. G. Imperial, P. D. Penev, Effects of sleep restriction on the human plasma metabolome. Physiol. Behav. 122, 25–31 (2013).
63. Defronzo RA, Simonson D, Ferrannini E, Barrett E. Insulin resistance: a universal finding in diabetic states.Bull Schweiz Akad Med Wiss.1981:223–238.
64. Reaven GM. Insulin resistance, the insulin resistance syndrome, and cardiovascular disease. Panminerva Medica. 2005;47:201–210.3
65. Filippin L.I., Teixeira V.N., da Silva M.P., Miraglia F., da Silva F.S. Sarcopenia: A predictor of mortality and the need for early diagnosis and intervention. Aging Clin. Exp. Res. 2015;27:249–254.
66. Goodpaster B.H., Park S.W., Harris T.B., Kritchevsky S.B., Nevitt M., Schwartz A.V., Simonsick E.M., Tylavsky F.A., Visser M., Newman A.B. The loss of skeletal muscle strength, mass, and quality in older adults: The health, aging and body composition study. J. Gerontol. A Biol. Sci. Med. Sci. 2006;61:1059–1064.
67. Jonatan R Ruiz, research associate,1,2 Xuemei Sui, research associate,3 Felipe Lobelo, research associate,3 James R Morrow, Jr, professor,4 Allen W Jackson, professor,4 Michael Sjöström, associate professor,1 and Steven N Blair, professor3,4.Association between muscular strength and mortality in men: prospective cohort study.BMJ. 2008 Jul 12; 337(7661): 92–95.
68. Williams MA, Haskell WL, Ades PA, Amsterdam EA, Bittner V, Franklin BA, et al. Resistance exercise in individuals with and without cardiovascular disease: 2007 update: a scientific statement from the American Heart Association Council on Clinical Cardiology and Council on Nutrition, Physical Activity, and Metabolism. Circulation 2007;116:572-84.
69. Thomis MA, Beunen GP, Maes HH, Blimkie CJ, Van Leemputte M, Claessens AL, et al. Strength training: importance of genetic factors. Med Sci Sports Exerc 1998;30:724-31.
70. Phillips P. Grip strength, mental performance and nutritional status as indicators of mortality risk among female geriatric patients. Age Ageing 1986;15:53-6.
71. Fujita Y, Nakamura Y, Hiraoka J, Kobayashi K, Sakata K, Nagai M, et al. Physical-strength tests and mortality among visitors to health-promotion centers in Japan. J Clin Epidemiol 1995;48:1349-59.
72. Metter EJ, Talbot LA, Schrager M, Conwit R. Skeletal muscle strength as a predictor of all-cause mortality in healthy men. J Gerontol A Biol Sci Med Sci 2002;57:B359-65.
73. Katzmarzyk PT, Craig CL. Musculoskeletal fitness and risk of mortality. Med Sci Sports Exerc 2002;34:740-4.
74. Gale CR, Martyn CN, Cooper C, Sayer AA. Grip strength, body composition, and mortality. Int J Epidemiol 2007;36:228-35.
75. Sasaki H, Kasagi F, Yamada M, Fujita S. Grip strength predicts cause-specific mortality in middle-aged and elderly persons. Am J Med 2007;120:337-42.
76. Al Snih S, Markides KS, Ray L, Ostir GV, Goodwin JS. Handgrip strength and mortality in older Mexican Americans. J Am Geriatr Soc 2002;50:1250-6. 3
77. Rantanen T, Volpato S, Ferrucci L, Heikkinen E, Fried LP, Guralnik JM. Handgrip strength and cause-specific and total mortality in older disabled women: exploring the mechanism. J Am Geriatr Soc 2003;51:636-41.
78. Lindstrom M, Isacsson SO, Merlo J. Increasing prevalence of overweight, obesity and physical inactivity: two population-based studies 1986 and 1994. Eur J Public Health. 2003; 13(4):306–312.
79. Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003; 289(1):76–79.
80. Zhang C, Rexrode KM, van Dam RM, Li TY, Hu FB. Abdominal obesity and the risk of all-cause, cardiovascular, and cancer mortality: sixteen years of follow-up in US women. Circulation. 2008; 117(13):1658–1667.
81. Chen G.C., Chen S.J., Zhang R., Hidayat K., Qin J.B., Zhang Y.S. et al. (2016) Central obesity and risks of pre- and postmenopausal breast cancer: a dose-response meta-analysis of prospective studies. Obes. Rev. 17, 1167–1177
82. Ma Y., Yang Y., Wang F., Zhang P., Shi C., Zou Y. et al. (2013) Obesity and risk of colorectal cancer: a systematic review of prospective studies. PLoS One 8, e53916.
83. Aune D., Navarro R.D., Chan D.S., Vingeliene S., Abar L., Vieira A.R. et al. (2015) Anthropometric factors and endometrial cancer risk: a systematic review and dose-response meta-analysis of prospective studies. Ann. Oncol. 26, 1635–1648
84. Wang F. and Xu Y (2014) Body mass index and risk of renal cell cancer: a dose-response meta-analysis of published cohort studies. Int. J. Cancer 135, 1673–1686
85. Genkinger J.M., Spiegelman D., Anderson K.E., Bernstein L., van den Brandt P.A., Calle E.E. et al. (2011) A pooled analysis of 14 cohort studies of anthropometric factors and pancreatic cancer risk. Int. J. Cancer 129, 1708–1717
86. Turati F., Tramacere I., La Vecchia C. and Negri E (2013) A meta-analysis of body mass index and esophageal and gastric cardia adenocarcinoma. Ann. Oncol. 24, 609–617
87. Schmid D., Ricci C., Behrens G. and Leitzmann M.F (2015) Adiposity and risk of thyroid cancer: a systematic review and meta-analysis. Obes. Rev. 16, 1042–1054
88. Li Z.M., Wu Z.X., Han B., Mao Y.Q., Chen H.L., Han S.F. et al. (2016) The association between BMI and gallbladder cancer risk: a meta-analysis. Oncotarget 7, 43669–43679
89. Hidayat K., Du X., Chen G., Shi M. and Shi B. (2016) Abdominal obesity and lung cancer risk: systematic review and meta-analysis of prospective studies. Nutrients 8,
90. Giovannucci E., Ascherio A., Rimm E.B., Colditz G.A., Stampfer M.J. and Willett W.C. (1995) Physical activity, obesity, and risk for colon cancer and adenoma in men. Ann. Intern. Med. 122, 327–334
91. Larsson S.C. and Wolk A (2007) Obesity and colon and rectal cancer risk: a meta-analysis of prospective studies. Am. J. Clin. Nutr. 86, 556–565
92. Pischon T., Lahmann P.H., Boeing H., Friedenreich C., Norat T., Tjonneland A. et al. (2006) Body size and risk of colon and rectal cancer in the European Prospective Investigation Into Cancer and Nutrition (EPIC). J. Natl. Cancer Inst. 98, 920–931
93. JURCA, R., M. J. LAMONTE, T. S. CHURCH, C. P. EARNEST, S. J. FITZGERALD, C. E. BARLOW, A. N. JORDAN, J. B.KAMPERT, and S. N. BLAIR. Associations of Muscle Strength and Aerobic Fitness with Metabolic Syndrome in Men. Med. Sci. Sports Exerc., Vol. 36, No. 8, pp. 1301–1307, 2004.
94. TREUTH, M. S., A. S. RYAN, R. E. PRATLEY, et al. Effects of strength training on total and regional body composition in older men. J. Appl. Physiol. 77:614–620, 1994.
95. HONKOLA, A., T. FORSEN, and J. ERIKSSON. Resistance training improves the metabolic profile in individuals with type 2 diabetes. Acta Diabetol. 34:245–248, 1997.
96. HURLEY, B. F., J. M. HAGBERG, A. P. GOLDBERG, et al. Resistive training can reduce coronary risk factors without altering VO2max or percent body fat. Med. Sci. Sports Exerc. 20:150–154, 1988.
97. MILLER, W. J., W. M. SHERMAN, and J. L. IVY. Effect of strength training on glucose tolerance and post-glucose insulin response. Med. Sci. Sports Exerc. 16:539–543, 1984.
98. M S Treuth 1 , G R Hunter, T Kekes-Szabo, R L Weinsier, M I Goran, L Berland.Reduction in intra-abdominal adipose tissue after strength training in older women.J Appl Physiol (1985). 1995 Apr;78(4):1425-31.
99. Hung-Ting Chen 1 , Yu-Chun Chung 2 , Yu-Jen Chen 3 , Sung-Yen Ho 4 , Huey-June Wu 4.Effects of Different Types of Exercise on Body Composition, Muscle Strength, and IGF-1 in the Elderly with Sarcopenic Obesity.J Am Geriatr Soc. 2017 Apr;65(4):827-832.
100. J M Jakicic 1 , K Clark, E Coleman, J E Donnelly, J Foreyt, E Melanson, J Volek, S L Volpe, American College of Sports Medicine.American College of Sports Medicine position stand. Appropriate intervention strategies for weight loss and prevention of weight regain for adults.Med Sci Sports Exerc. 2001 Dec;33(12):2145-56.
101. Sivertsen H, Bjørkløf GH, Engedal K, Selbæk G, Helvik A. Depression and quality of life in older persons: A review. Dementia and Geriatric Cognitive Disorders. 2015;40(5–6):311–339.
102. Chachamovich E, Fleck M, Laidlaw K, Power M. Impact of major depression and subsyndromal symptoms on quality of life and attitudes toward aging in an international sample of older adults. The Gerontologist. 2008;48
(5):593–602.
103. Castro-Costa E, Dewey M, Stewart R, Banerjee S, Huppert F, Mendonca-Lima C, et al. Prevalence of depressive symptoms and syndromes in later life in ten European countries: The SHARE study. The British Journal of
Psychiatry: The Journal of Mental Science. 2007
104. Eriksson M, Lindström B. Antonovsky’s sense of coherence scale and the relation with health: A systematic review. Journal of Epidemiology and Community Health. 2006
105. Rejeski WJ, Mihalko SL. Physical activity and quality of life in older adults. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2001;56(2):23–35.
106. Netz Y, Wu MJ, Becker BJ, Tenenbaum G. Physical activity and psychological well-being in advanced age: A meta-analysis of intervention studies. Psychology and Aging. 2005;20(2):272–284.
107. Gillison FB, Skevington SM, Sato A, Standage M, Evangelidou S. The effects of exercise interventions on quality of life in clinical and healthy populations; a meta-analysis. Social Science & Medicine. 2009
108. Rhyner KT, Watts A. Exercise and depressive symptoms in older adults: A systematic meta-analytic review. Journal of Aging and Physical Activity. 2016
109. O’Connor PJ, Herring MP, Caravalho A. Mental health benefits of strength training in adults. American Journal of Life style Medicine. 2010;4(5):377–396. doi: 10.1177/1559827610368771. [CrossRef] [Google Scholar]
110. Dunn AL, Trivedi MH, O’Neal HA. Physical activity dose-response effects on outcomes of depression and anxiety. Medicine and Science in Sports and Exercise. 2001;33:S587–S597.
111. Chien-Ning Tseng 1 , Bih-Shya Gau, Meei-Fang Lou.The effectiveness of exercise on improving cognitive function in older people: a systematic review.J Nurs Res. 2011 Jun;19(2):119-31.
112. Nakamoto H, Yoshitake Y, Takai Y, Kanehisa H, Kitamura T, Kawanishi M, Mori S. Knee extensor strength is associated with mini-mental state examination scores in elderly men. Eur J Appl Physiol. 2012;112:1945–1953.
113. Chen W-L, Peng T-C, Sun Y-S, Yang H-F, Liaw F-Y, Wu L-W, et al. Examining the association between quadriceps strength and cognitive performance in the elderly. Medicine (Baltimore) 2015;94:e1335.
114. Frith E, Loprinzi PD. The association between lower extremity muscular strength and cognitive function in a national sample of older adults. J Life style Med. 2018;8:99–104.
115. Steves CJ, Mehta MM, Jackson SHD, Spector TD. Kicking back cognitive ageing: leg power predicts cognitive ageing after ten years in older female twins. Gerontology. 2016;62:138–149.
116. Pentikäinen H, Savonen K, Komulainen P, Kiviniemi V, Paajanen T, Kivipelto M, et al. Muscle strength and cognition in ageing men and women: the DR’s EXTRA study. Eur Geriatr Med. 2017;8:275–277.
117. Forte R, Boreham CAG, Leite JC, de Vito G, Brennan L, Gibney ER, Pesce C. Enhancing cognitive functioning in the elderly: multicomponent vs resistance training. Clin Interv Aging. 2013;8:19–27.
118. Coetsee Carla, Terblanche Elmarie. Cerebral oxygenation during cortical activation: the differential influence of three exercise training modalities. A randomized controlled trial. European Journal of Applied Physiology. 2017;117(8):1617–1627.
119. Nagamatsu LS, Handy TC, Hsu CL, Voss M, Liu-Ambrose T. Resistance training promotes cognitive and functional brain plasticity in seniors with probable mild cognitive impairment. Arch Intern Med. 2012;172:666–668.
120. Tsai C-L, Ukropec J, Ukropcová B, Pai M-C. An acute bout of aerobic or strength exercise specifically modifies circulating exerkine levels and neurocognitive functions in elderly individuals with mild cognitive impairment. Neuroimage Clin. 2018;17:272–284.
121. Fiatarone Singh MA, Gates N, Saigal N et al. The Study of Mental and Resistance Training (SMART) study—resistance training and/or cognitive training in mild cognitive impairment: A randomized, double-blind, double-sham controlled trial. J Am Med Dir Assoc 2014;15:873–880.
122. J N Nielsen 1 , E A Richter.Regulation of glycogen synthase in skeletal muscle during exercise.Acta Physiol Scand. 2003 Aug;178(4):309-19.











